|
|
 |
 |
 HOME > 증 례 002 HOME > 증 례 002 |
|
On occasion, Andersson lesion is misdiagnosed as infectious spondylitis such as tuberculous spondylitis. This case was initially misdiagnosed as tuberculous spondylitis by radiologists, too, but we believed that it was not an infectious disorder because of three MRI findings. First, the anterior longitudinal ligament was intact: there was neither transligamentous nor subligamentous extension of the lesion. Second, there was no paravertebral abscess. Third, if it were infection, it would have spread cephalocaudally in the epidural space once it had invaded into that space, because there is actually no barrier to the spread in this space. However, in this case, the epidural invasion of the lesion was relatively minimal, even though it involved interspinous ligament.
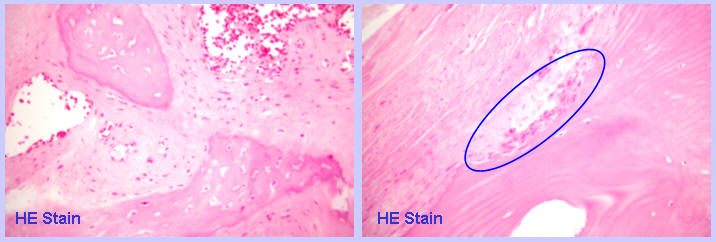
To differentiate from infectious conditions, open biopsy of the interspinous ligament area was performed first. Using a straight osteotome, the ligament and the adjacent spinous processes were removed en bloc in a wedge-shape. On removal of this wedge, a clean loose connective tissue appeared deep to the ligament, while pus, discharges, or infected granulation tissues were not found at all. On light microscopic examination with hematoxylin and eosin (HE) staining, fibro-vascular granulation tissues and osteolytic activity was observed, but inflammatory cell infiltration were not observed.
|
|
 |
Posterior decompression and fusion of the T11-12 with pedicle screw instrumentation of T10-L1 was performed. A fibro-osseous lesion consisting of old scar-like hypertrophic connective tissues, thickened laminae, and osteophytes compressing the spinal cord was removed from the T11-12 inter-laminar space. The spine was instrumented and stabilized in a naturally extended position, and bone grafting was carried out.
Seven days later, anterior fusion of T11-12 was performed. The disc was found to be partially replaced by the same clean loose connective tissues as were found during the posterior surgery. No infected tissues such as pus, discharges, or infected granulation tissues were found. An iliac strut graft was firmly inserted into the T11-12 disc space, and a morsellized rib graft was inserted between the iliac strut and the anterior longitudinal ligament.
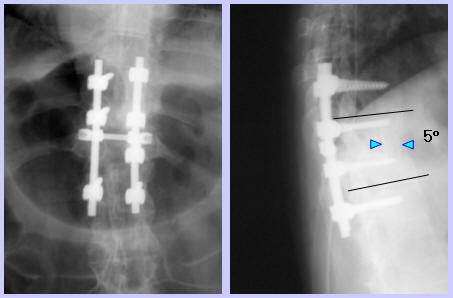
The postoperative course of the patient was uneventful. On the day after the posterior surgery, ankle clonus disappeared and partial subsidence of the sensory disturbances was noted. Neurologic disturbances were progressively reduced, and at the last follow-up at 24 months after the surgeries, ankle clonus was absent, deep tendon reflexes and muscle power of the lower extremities were normal, touch and position sensation was almost normal, and the gait was almost normal, too. Back pain was much improved, and he felt mild back discomfort only in the morning. On simple roentgenograms, the anterior bone block seemed to be collapsed and the spine was fused in a flexed position. However, bone union was complete and he felt no disability or discomfort associated with mild kyphosis which had preoperatively existed in standing position.
|
|
 |
Andersson lesion is sterile spondylodiscitis or pseudarthrosis rarely occurring in ankylosing spondylitis patients. It is characterized by osteolysis, sclerosis and absence of syndesmophytes. This lesion is usually asymptomatic, and the symptom, if any, is usually back pain, which usually is mild. Prognosis is reported to be good with conservative treatment including NSAID's, rest, and physiotherapy, and spinal fusion is rarely indicated. To our knowledge, only one case of myelopathy caused by Andersson lesion is reported in the English literature: in this case the lesion was located in the cervical vertebrae. Therefore, to the best of our knowledge, this is the first case of Andersson lesion which caused myelopathy in the thoracic spine, which is more stable than the cervical spine.
Most patients with Anderson lesions have no history of trauma, as in this case, or only minor trauma. Two mechanisms have been proposed that contribute to these lesions: mainly inflammatory like increasing enthesopathy, and mainly mechanical like a fatigue fracture or pseudarthrosis in the stiffened axial skeleton. This case showed no inflammatory reaction on either gross finding or on histological examination, and is inferred as pseudarthrosis of a fatigue fracture. In this case, dynamic compression by severe segmental instability revealed by flexion/extension lateral radiographs was thought to have played an important role in the development of myelopathy as well as static compression by hypertrophic fibro-osseous tissues shown in static MR/CT images. Decompression and solid fusion was mandatory in this case, and resulted in an excellent recovery from both neurologic deficits and back pain. We regret instrumenting only 2 levels above and below in an area with high stress concentration and with relatively weak bone which resulted in union in a flexed position. Fortunately, however, fusion was solid and he complained of nothing associated with it.
<Back>
|
|
|
|


