|
|
 |
 |
 HOME > 증 례 002 HOME > 증 례 002 |
|
This 49-year-old man was admitted with a one-year history of progressive gait disturbance with motor weakness, spasticity, and sensory disturbances in the lower extremities. He had an about 20-year history of back pain, which had been aggravated since 3 years prior to admission. His back pain, however, was not so severe that he had just needed NSAID medication and physiotherapy. He was diagnosed as ankylosing spondylitis about 8 years prior to admission. He denied any history of trauma.
The knee and ankle jerks were hyperactive, and unsustained ankle clonus was noted on both sides. The muscle power grades of the lower extremities were around four. Proprioception was almost absent on both lower extremities, and touch sensation was markedly diminished below the T12 level. Incoordination of the lower limb muscles along with deficient proprioception were thought to be the main cause of gait disturbance. His WBC count, ESR, and CRP were 6100/mm3, 119 mm/hr, and 2+/4.15 respectively.
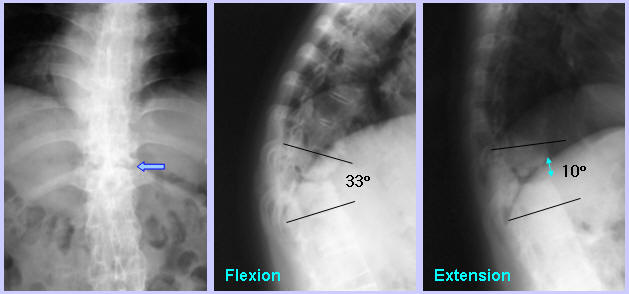
On simple roentgenograms, syndesmophyte was not observed in the T11-12 interspace. The inferior endplate of T11 was severely destructed, while the superior endplate of T12 seemed to be relatively preserved. While flexion lateral view showed narrowing of T11-12 disc space, which, along with severe destruction of anteroinferior portion of the T11 body, caused marked local kyphosis, extension lateral view showed remarkable widening of T11-12 disc space. Thus, the T11-12 was hypermobile or unstable.
MRI revealed a soft tissue lesion extending from the T11-12 disc space and the adjacent vertebral bodies to the interspinous and supraspinous ligament, which was compressing the spinal cord. CT scan revealed that osteophytes growing from the thickened lamina also played a role in spinal cord compression in addition to the soft tissue lesion seen on MRI.

<Question>
What is the diagnosis and treatment?
<Answer>
|
|
|
|


